Human papilloma viruses – you don’t see them, you don’t feel them, and yet they are often our long-time companions
The human papillomavirus (HPV) is a virus that can cause, among other things, anogenital warts (so-called condylomas) and changes in the cervix in women. These changes can develop over months or years into precancerous lesions and eventually into cervical cancer (so-called cervical carcinoma).
There are more than 100 different HPV subtypes, some of which are high-risk types with a high potential for change and others are low-risk types with a low cancer-causing potential.
Human papillomavirus DNA could be detected in 99.7% of all cervical carcinomas – a fact that shows that cervical cancer can hardly develop without HPV infection. The link between persistent HPV infection with a high-risk HPV type and the risk of developing cervical cancer has been scientifically proven many times and is generally accepted.
It is estimated that more than 80% of sexually active adults acquire an HPV infection at least once in their lifetime. This makes HPV the most common sexually transmitted infection.
HPV is transmitted through oral, vaginal or anal sex. However, infection can also occur through contact with the skin or mucous membranes of an infected person. Therefore, condoms reduce the risk of transmission, but cannot eliminate it completely. Human papilloma viruses are so highly contagious that even consistent safer sex does not offer complete protection against infection.
Regular gynaecological screening can help to detect such HPV-related precancerous lesions in time and thus prevent the development of cervical cancer. Regular gynaecological screening and HPV vaccination are the most important elements in the prevention of cervical cancer.

Currently, an HPV vaccine is used that covers the 2 HPV types that most commonly cause condylomas and the 7 high-risk types that are most often responsible for the development of precancerous lesions and cervical cancer. Vaccination is paid for up to the age of 26 as part of the cantonal vaccination programmes. After the age of 26, coverage depends on health insurance, but supplementary insurance often covers part of the vaccination costs. In certain situations, HPV vaccination can still be recommended after treatment of a precancerous lesion, as studies have shown that this can lead to a decrease in the recurrence rate. There is no approval for vaccination against HPV during pregnancy. However, the HPV vaccine is an inactivated vaccine with no risk of teratogenic effects on the fetus.
Why can human papillomaviruses be so dangerous?
Human papillomaviruses infect the cells of the so-called transformation zone of the cervix. This zone is characterised by multi-layered squamous epithelium gradually changing into glandular epithelium through the transformation process of metaplasia. The cells of this area are very susceptible to HPV carcinogenesis, but at the same time show a high potential for spontaneous healing. Thus, about 80-90% of HPV infections disappear within a period of up to 2 years. Even infections that have already led to cell changes are still successfully fought by the immune system and heal. A persistent infection of the cervix with an HPV high-risk type for many years is the necessary prerequisite for the development of a so-called intraepithelial neoplasia (SIL/CIN). Additional factors that favour the development of cancer are smoking, a young childbearing age, the use of oral contraceptives for more than 5 years, a simultaneous infection with other sexually transmitted pathogens (such as chlamydia) and a weakened immune system (e.g. due to stress).
What happens during the cervical cancer screening examination?
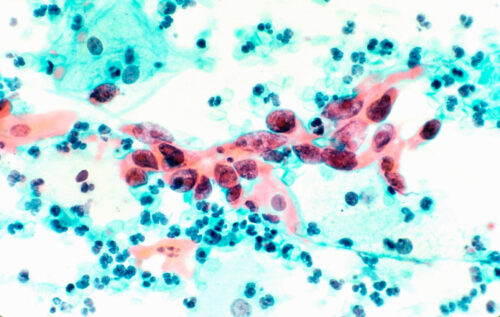
In Switzerland, it is recommended to start cervical cancer screening from the age of 21, regardless of whether you have started sexual activity or other risk factors. During the examination, your doctor will take a cytological smear (known as a PAP smear) from the transformation zone of the cervix. The cells taken will be sent to the cytology laboratory where they will be assessed under the microscope. If no cells from the transformation zone are found in the cytological smear, it is not representative and it is recommended to repeat the smear. If risk factors are present (e.g. conspicuous smear in the medical history), this should be done within 3-6 months if possible.

My Pap smear is abnormal – what does that mean for me now?
Abnormalities in the cytological smear are often detected and are usually not cause for concern. It simply means that something in the smear is not right and a more detailed check is needed. Depending on the smear result, your doctor will make one of the following recommendations.
- Repeat the cytological smear test e.g. after 6 and 12 months: this may be recommended for mild changes where spontaneous normalisation of the smear test is very common. Mild changes do not necessarily have to do with precancerous lesions, but can also be caused reactively by a vaginal infection with bacteria or fungi. In such a situation, local vaginal treatment with vaginal tablets is often recommended, followed by a repeat Pap smear.
- Performing an HPV test: this test can be performed directly on the smear material and provides information on whether an infection with an HPV high-risk type is present.
- Performing a colposcopy: during this examination, your doctor will look at the cervix with a colposcope (similar to a microscope). The cervix is dabbed with special solutions that make small changes visible and can thus indicate a precancerous condition. Such an abnormality can be specifically biopsied in the same examination.
Overview of common abnormal smear results and their consequences
- NILM: inconspicuous smear result
Cells of squamous origin:
- ASC-US: Atypical squamous cells of undetermined significance
- ASC-H: Atypical squamous cells cannot exclude HSIL
- LSIL: Low-grade squamous intraepithelial lesion = mild change
- HSIL: High-grade squamous intraepithelial lesion = medium- or higher-grade change
Cells of glandular origin:
- AGC-NOS: Atypical glandular cells, not otherwise specified
- AGC-FN: Atypical glandular cells, favor neoplasia
Procedure for ASC-US and ASC-H
ASC changes are divided into “atypical cells of undetermined significance” (ASC-US) and “atypical cells in which a high-grade squamous epithelial lesion cannot be excluded” (ASC-H).
- ASC-US:
The further procedure for an ASC-US depends on the age of the patient. If the patient is 30 years of age or older, there are 2 ways to proceed. First, HPV typing can be carried out to determine whether an infection with one of the known HPV high-risk types is present. If infection with an HPV high risk type is detected in a woman with ASC-US, a colposcopy and, if necessary, a targeted biopsy should be performed. If the HPV test is negative, the risk of a precancerous lesion is so low that it is sufficient if the cytological smear is repeated after one year. In most cases, the smear normalises itself within this time. Another possible procedure for patients with ASC-US who are older than 30 years is to repeat the cytological smear after 6 and 12 months. If both cytological smears are unremarkable, it is possible to return to the regular check-ups as part of preventive care. If the smear result does not normalise, a colposcopy is recommended.
HPV typing is not recommended for women under 30 years of age, because HPV infections occur so frequently at this age and in most cases disappear on their own, so that no specific consequences would result from the test result. It is therefore recommended in these patients to perform a repeat smear test after 6 and 12 months with ASC-US. If both smear tests are inconspicuous, regular screening controls can be continued again.
- ASC-H:
With these changes, a medium- or higher-grade lesion may be present, so that further clarification should be carried out by means of colposcopy. This examination involves looking at the cervix with a colposcope (similar to a microscope). By applying special solutions (usually vinegar and iodine solution), small changes can be made visible that indicate a precancerous lesion. Such an abnormality can then be specifically biopsied with a small forceps in the same examination. The removal of tissue is not painful.
Procedure for LSIL
This smear result is usually a case of mild changes. If an infection with an HPV high-risk type is known or if it is not known whether an infection with an HPV high-risk type is present, a colposcopy should be performed. If there is a negative HPV test, the cytological smear and the HPV test can be repeated after one year. In patients younger than 30 years, no HPV test should be performed. In this case, it is recommended to repeat the smear test after 6 and 12 months.

Procedure for HSIL
This is a smear test result in which moderate to severe cell changes are present. The risk of pre-cancer is up to 70% and the risk of cervical cancer is up to 7%. If you have such a smear result, the next step should be a colposcopy with biopsy. By taking the tissue sample, the precancerous stage can be confirmed and appropriate treatment can be initiated. In this case, your doctor will usually recommend a so-called conisation, in which the diseased tissue is removed using the loop technique (LEEP). In very young women, the indication for conisation is somewhat more cautious because of the very high chance of spontaneous healing. In addition, conisation is associated with a slightly increased risk of premature birth in later pregnancies.
Abnormal glandular cells: AGC-NOS and AGC-FN
If you have been diagnosed with such a smear result, it is abnormal glandular cells in the findings. Glandular cells are found in the cervical canal and in the uterine cavity. A colposcopy and a transvaginal sonography should be recommended for this smear test. If certain risk factors are present (e.g. age > 35 years, a positive family history for corresponding cancers or the presence of bleeding disorders or bleeding after menopause), a uterus endoscopy with scraping of the endometrium should also be performed.
What does CIN mean?
The abbreviation CIN stands for cervical intraepithelial neoplasia and also describes cell changes (dysplasias) on the cervix that are considered precursors to cervical cancer. However, the diagnosis of CIN is not only made by a cytological smear test, but by examining a tissue sample (biopsy) from the cervix. There are 3 different stages of cervical intraepithelial neoplasia:
- CIN I: low-grade dysplasia
- CIN II: medium-grade dysplasia
- CIN III: high-grade dysplasia
If the doctor finds a cervical intraepithelial neoplasia, this is not usually a cause for concern. Many of these cell changes regress spontaneously within 1-2 years. The likelihood that the CIN will disappear on its own depends on the extent and duration of the HPV infection. The longer an infection with an HPV high-risk type has existed, the less likely spontaneous regression is.
CIN I involves mild cell changes. It heals spontaneously without treatment in 60% of cases. 10% of all CIN I cases develop over several years into CIN III. If you have CIN I, your doctor will check every 3 months by means of a cytological smear test to see whether the cell changes are regressing. If CIN I has been present for more than 2 years, he/she will recommend conisation.
CIN II describes a moderately severe form of cell changes. In 40% of cases, it heals on its own within 2 years. In 20% of cases, it develops into CIN III. If you have been diagnosed with CIN II, it does not have to be treated immediately. Follow-up checks should be carried out every 3 months by means of a cytological smear test to check how the CIN II develops. If the cell changes have not disappeared after one year, you will be recommended a conisation.
In the case of CIN III, the cell changes are already more advanced, so that the chance of spontaneous regression is only slight. With this finding, it is very likely that the dysplasia will turn into cervical cancer. Your doctor will therefore advise you to have a conisation in this situation without waiting any longer.
Do you have any further questions about HPV infections and gynaecological screening or have you been diagnosed with an abnormal Pap smear? We will be happy to advise you in a personal consultation.
Would you like to learn more about HPV and the HPV vaccination? Visit our HPV website at www.hpv-shield.ch

FMH for gynaecology and obstetrics
More on the subject: Walking the talk: Lunch & Learn über HPV

